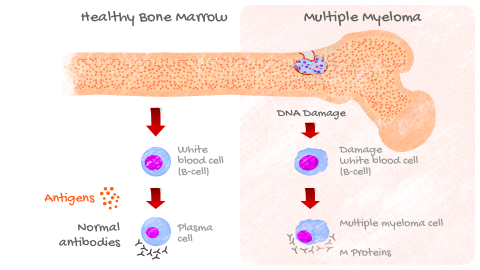
Multiple myeloma is a type of blood cancer that forms in the bone marrow – the soft spongy part of your bone. It is the second most common type of blood cancer after lymphoma.
Bone marrow contains many cells including red blood cells and a special type of cell called plasma cells. Healthy plasma cells are responsible for producing antibodies to fight infections.
In multiple myeloma, plasma cells become cancerous and accumulate rapidly crowding out:
- Red blood cells which are necessary to carry oxygen to the tissues in your body.
- White blood cells which are needed to fight infection and disease.
- Platelets which help your blood clot.
These cancer cells also produce high levels of an abnormal protein called M protein, which can cause other complications.
There are 2 main types of multiple myeloma:
- Inactive smoldering myeloma.
- Active multiple myeloma.
If you don’t respond to treatment or the disease returns after treatment then you may have relapsed/refractory multiple myeloma.
References:
- What Is Multiple Myeloma? | The MMRF.” Themmrf.Org, https://themmrf.org/multiple-myeloma/. Accessed 7 Apr. 2022.
- Multiple Myeloma - NCIS | National University Cancer Institute, Singapore. https://www.ncis.com.sg/Cancer-Information/About-Cancer/Pages/Multiple-Myeloma.aspx. Accessed 7 Apr. 2022.
- “What Are MGUS, Smoldering Multiple Myeloma, and Active Myeloma?” International Myeloma Foundation, https://www.myeloma.org/what-are-mgus-smm-mm. Accessed 7 Apr. 2022.
You may have multiple myeloma if you have the C.R.A.B features.
Consult your primary care doctor if you notice these signs and symptoms.
If he/she suspects you have multiple myeloma, you will be referred to a hematologist.
Calcium levels are increased
- Trouble thinking clearly, confusion
- Feeling thirsty
- Constipation
- Excessive urination
- Loss of appetite
- Nausea
- Weakness
- Arrhythmias
Renal failure
- Trouble thinking clearly, confusion
- Feeling thirsty
- Nausea/ vomiting
- Changes in urination
- Fatigue, sleep problems
- Cramps
- Breath odour
- Shortness of breath
- Easy bruising or bleeding

Anemia
- Easy fatigue
- Loss of energy
- Rapid heartbeat, especially with exercise
- Shortness of breath

Bone damage
Shortness of breath
Lytic bone lesions
Broken bones
Hypercalcemia
Spinal cord compression (causing extremity numbness, bladder and/or bowel dysfunction and sometimes paralysis
Other symptoms include recurrent infections and fevers resulting from reduction in the number of normal healthy immune cells which produce antibodies to fight infection and bruising or bleeding early from the reduced number of platelets that help in clotting.
References:
- “Multiple Myeloma - Symptoms and Causes.” Mayo Clinic, https://www.mayoclinic.org/diseases-conditions/multiple-myeloma/symptoms-causes/syc-20353378. Accessed 7 Apr. 2022.
- “Common Symptoms of Multiple Myeloma | The MMRF.” Themmrf.Org, https://themmrf.org/multiple-myeloma/symptoms-and-side-effects/. Accessed 7 Apr. 2022.
- “Multiple Myeloma - Stages.” Cancer.Net, 25 June 2012, https://www.cancer.net/cancer-types/multiple-myeloma/stages.
- Multiple Myeloma - NCIS | National University Cancer Institute, Singapore. https://www.ncis.com.sg/Cancer-Information/About-Cancer/Pages/Multiple-Myeloma.aspx. Accessed 7 Apr. 2022.
Multiple myeloma is a clonal disease. Each person is unique with different populations of cancer cells caused by different genetic mutations. But it is NOT a hereditary disease that is passed down in families.
Multiple myeloma almost always starts as monoclonal gammopathy of undetermined significance (MGUS).
Abnormal M proteins are present in very low amounts in MGUS, but there are no features of multiple myeloma. The risk of progression to symptomatic multiple myeloma in MGUS patients is 1% per year. It usually progresses to an intermediate smoldering multiple myeloma to active multiple myeloma.
The exact cause of multiple myeloma is not known, but a few risk factors have been identified.
ARE YOU AT RISK FOR MULTIPLE MYELOMA?

INCREASING AGE:
Risk of multiple myeloma increases with age. If you are over the age of 55, you may be at risk.

MALE SEX:
Men are more likely to develop multiple myeloma than women.

PERSONAL HISTORY OF MONOCLONAL GAMMOPATHY OF UNDETERMINED SIGNIFICANCE (MGUS):
Get your M protein levels checked regularly to see if you are progressing.

MULTIPLE MYELOMA:
If a family member or close relative had multiple myeloma you could be at risk.
References:
- “Multiple Myeloma Diagnosis | The MMRF.” Themmrf.Org, https://themmrf.org/multiple-myeloma/diagnosis/. Accessed 7 Apr. 2022.
- Multiple Myeloma - NCIS | National University Cancer Institute, Singapore. https://www.ncis.com.sg/Cancer-Information/About-Cancer/Pages/Multiple-Myeloma.aspx. Accessed 7 Apr. 2022.
Correct diagnosis of multiple myeloma is important. It helps your doctor to stage your disease, determine your prognosis and decide the correct treatment options.
A range of diagnostic tests help to assess the extent of the disease including:

BLOOD TESTS:
- To determine if there are elevated levels of proteins including M protein, antibodies, albumin, lactate dehydrogenase (LDH) and beta-2 macroglobulin (β2-M)
- To examine kidney function, check blood cell counts, calcium and uric acid levels

URINE TESTS:
- To determine the level of a specific type of M protein called Bence Jones proteins which may clog the kidneys and signify kidney damage due to multiple myeloma.

GENETIC TESTS:
- To determine if there are abnormal changes in the DNA chromosomes using a technique called Fluorescence In-Situ Hybridization (FISH) or the presence of individual gene mutations

IMAGING TESTS:
- To determine the presence of bone damage and to look for the number and size of tumors in bone. These include X-ray, MRI, CT and PET scans
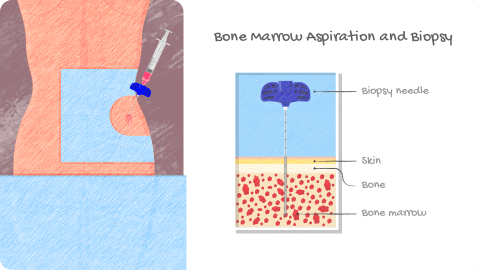
BONE MARROW ASPIRATION AND BIOPSY
Confirmation of a multiple myeloma diagnosis is usually done through a bone marrow biopsy. It is normally a 30-45 minute outpatient procedure.
-
WHAT DOES YOUR DOCTOR LOOK FOR?
This procedure examines tissue from bone marrow for the number and percentage of normal vs cancer cells. A higher percentage of myeloma cells indicates advanced disease.
-
HOW IS IT PERFORMED?
A small area of skin will be numbed usually around your hip bone or other large bone. A thick hollow needle is inserted into the bone and a sample of blood, bone and bone marrow is taken for analysis.
What to expect?
BEFORE
THE PROCEDURE
Bone marrow biopsies carry a risk of bleeding. Be sure to tell your doctor if you are on any pain medications (aspirin, ibuprofen) or on blood thinners. If you are allergic to anesthesia please inform the doctor
DURING
THE PROCEDURE
Some people experience pain during the procedure. If you are anxious about the procedure, talk to your doctor about your options to relive pain (medications/intravenous sedation)
AFTER
THE PROCEDURE
Biopsy area may feel sore for several days. Inform your doctor if you see the any of the following signs of an infection or complication – fever, bleeding or discharge, increased pain, other signs of infection
References:
- “NCCN Guidelines® Insights: Multiple Myeloma, Version 3.2022: Featured Updates to the NCCN Guidelines.” Journal of the National Comprehensive Cancer Network, vol. 20, no. 1, Jan. 2022, pp. 8–19.
- Bone marrow aspiration and biopsy. Cancer.net. Dec 2019. https://www.cancer.net/navigating-cancer-care/diagnosing-cancer/tests-and-procedures/bone-marrow-aspiration-and-biopsy
After you are diagnosed, your doctor will classify your disease into stages.
You may also be assigned a risk category (standard or high risk) to indicate how aggressive your multiple myeloma is.
To choose the right treatment option as well as to assess response to treatment, your doctor may perform additional cytogenetic tests.
These tests look for abnormalities in the chromosomes that carry genes, causing them to make too many or too few proteins. These could be deletions or additions to chromosomes or swapping of parts of different chromosomes.
Multiple myeloma stages
Your doctor may use a Revised International Staging System (R-ISS) to help classify your disease. It is based on measurement of four parameters

- β2-M less than 3.5 mg/L
- Serum albumin of 3.5 g/dL or more
- Normal LDH
- No high-risk chromosome changes in myeloma cells found by FISH test

- Not stage I or stage III

- β2-M is more than 5.5 mg/L
- High risk cytogenetics or elevated serum LDH
References:
- “Multiple Myeloma - Stages.” Cancer.Net, 25 June 2012, https://www.cancer.net/cancer-types/multiple-myeloma/stages.
- Joshua DE, Bryant C, Dix C, Gibson J, Ho J. Biology and therapy of multiple myeloma. Med J Aust. 2019;210(8):375-380.
- “NCCN Guidelines® Insights: Multiple Myeloma, Version 3.2022: Featured Updates to the NCCN Guidelines.” Journal of the National Comprehensive Cancer Network, vol. 20, no. 1, Jan. 2022, pp. 8–19.