Currently, there is NO CURE for multiple myeloma.
But there is HOPE.
New treatment options are available that can help prolong life and keep multiple myeloma under control, reduce and stop the symptoms for a longer period of time.
There is no single recommended treatment for multiple myeloma. Your doctor will work with you to develop a treatment plan that depends on:
- Stage of the disease
- Age at the time of treatment
- Overall health status
- And your preferences
In some cases, when you are at early stages of the disease, your doctor may recommend “watchful waiting” to avoid the side effects of cancer treatment.
With regular 3-month check-ups your doctor will help you decide when is the right time to start treatment.

References:
- NCCN Guidelines® Insights: Multiple Myeloma, Version 3.2022: Featured Updates to the NCCN Guidelines.” Journal of the National Comprehensive Cancer Network, vol. 20, no. 1, Jan. 2022, pp. 8–19.
- Multiple Myeloma - NCIS | National University Cancer Institute, Singapore. https://www.ncis.com.sg/Cancer-Information/About-Cancer/Pages/Multiple-Myeloma.aspx. Accessed 7 Apr. 2022.
If you are diagnosed with multiple myeloma, you are likely to be treated with a combination of drugs that work in different ways to target the myeloma cells in your body.
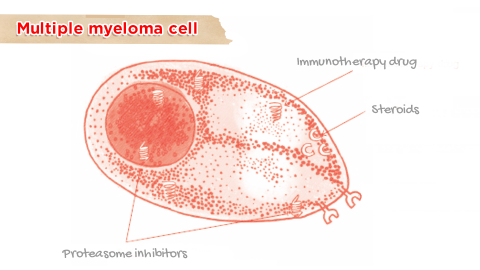
The standard treatment is a TRIPLET THERAPY involving a combination of three medicines

A proteasome inhibitor (disposes damaged proteins)

An immunotherapy drug (boosts the immune system)

A corticosteroid (has anti-cancer effects)
Some patients may also receive four treatments or may be eligible for a stem cell transplant.
You may also receive treatments to help relieve some of the symptoms of myeloma and side effects associated with treatment.
Some of these treatment options specifically target abnormal proteins or certain growth signals that are responsible for the growth of the myeloma cells and are called TARGETED THERAPIES.
References:
- “NCCN Guidelines® Insights: Multiple Myeloma, Version 3.2022: Featured Updates to the NCCN Guidelines.” Journal of the National Comprehensive Cancer Network, vol. 20, no. 1, Jan. 2022, pp. 8–19.
- “Standard Treatments for Multiple Myeloma | The MMRF.” Themmrf.Org, https://themmrf.org/multiple-myeloma/treatment-options/standard-treatments/. Accessed 7 Apr. 2022.
There are many different types of targeted therapies. For example:

PROTEASOME INHIBITOR
These are drugs that target proteosomes which are complexes that dispose old and damaged proteins. They cause myeloma cells to die by preventing them from removing damaged proteins.

STEROIDS
Some steroids have anti-cancer effects and are often used in combination with other targeted therapies.
Immunotherapy drugs
These drugs help to boost the body’s immune system. Depending on the proteins they activate/inhibit they are categorised as:

IMMUNOMODULATORS
These activate certain immune cells or prevent growth signals to myeloma cells

HDAC INHIBITORS
These block the action of certain enzymes which help in growth and survival of myeloma cells

MONOCLONAL ANTIBODIES
These are man-made antibodies that target specific proteins on the surface of myeloma cells

NUCLEAR EXPORT INHIBITORS
These prevent proteins from leaving the nucleus of a myeloma cell, thereby stopping it from functioning
References:
- “Standard Treatments for Multiple Myeloma | The MMRF.” Themmrf.Org, https://themmrf.org/multiple-myeloma/treatment-options/standard-treatments/. Accessed 7 Apr. 2022.
- “NCCN Guidelines® Insights: Multiple Myeloma, Version 3.2022: Featured Updates to the NCCN Guidelines.” Journal of the National Comprehensive Cancer Network, vol. 20, no. 1, Jan. 2022, pp. 8–19.
Chemotherapy drugs or referred simply as “chemo” sometimes are non-specific unlike targeted therapy.
- Chemotherapy can be very good at getting rid of cancer cells in the body. They work by killing cells that are “fast-growing” within the body, those that are in the process of dividing rapidly. Cancer cells normally grow faster than normal healthy cells. The downside is some normal cells can get affected too. That is why you experience side effects. But these are largely manageable.
- Chemotherapy is often combined with targeted therapies or steroids. It is also commonly used in preparation for a stem cell transplant.
- If you do not have access to standard targeted triple therapy, experience side effects (peripheral neuropathy) from targeted therapy regimens or if you have impaired renal function your doctor may replace one of the drugs with chemotherapy.
Radiation therapy or irradiation is a type of local therapy. It is opted when cancer cells are localized in one area of the body.
- Radiation therapy uses high-energy particles or rays to destroy cancer cells and prevent them from growing, much in the same way as chemotherapy drugs work. Low-dose local irradiation is often used to treat bone lesions or a single group of myeloma cells, to relieve uncontrolled pain and prevent or treat bone fractures.
References:
- “NCCN Guidelines® Insights: Multiple Myeloma, Version 3.2022: Featured Updates to the NCCN Guidelines.” Journal of the National Comprehensive Cancer Network, vol. 20, no. 1, Jan. 2022, pp. 8–19.
- “Standard Treatments for Multiple Myeloma | The MMRF.” Themmrf.Org, https://themmrf.org/multiple-myeloma/treatment-options/standard-treatments/. Accessed 7 Apr. 2022.
Stem cell transplant (SCT) or bone marrow transplant is an alternative treatment for multiple myeloma.
SCT aims to replace the harmful myeloma cells with healthy blood-forming stem cells. These stem cells are specialized cells that are able to make many different types of blood cells.
The stem cells can help replace the red blood cells, white blood cells and platelets in the bone marrow, which are being crowded out by myeloma cells.
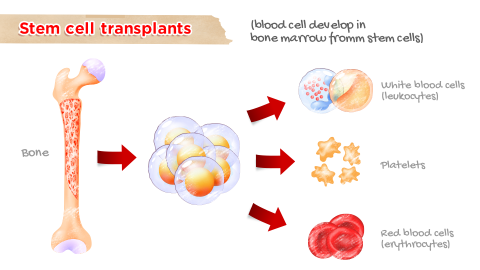
You may receive stem cells extracted from your own body (autologous SCT) or from an another donor (allogenic SCT). Before receiving a stem cell transplant, a high-dose of chemotherapy is used to kill as many myeloma cells as possible.
References:
- “NCCN Guidelines® Insights: Multiple Myeloma, Version 3.2022: Featured Updates to the NCCN Guidelines.” Journal of the National Comprehensive Cancer Network, vol. 20, no. 1, Jan. 2022, pp. 8–19.
- “Stem Cell Transplants for Multiple Myeloma | The MMRF.” Themmrf.Org, https://themmrf.org/multiple-myeloma/treatment-options/stem-cell-transplants/. Accessed 7 Apr. 2022.
All of the treatment options for multiple myeloma have some side effects, for example, fatigue, weakness and drowsiness.
These depend on the drug, the dosage and the person’s response to the medications
Some side effects can be very serious, while others are uncomfortable but not serious.
Most of the side effects will disappear when treatment is stopped, while some may be long-term or even appear several years later.
Talk to your doctor to understand what side effects to expect and how they can be managed.
Most common side effects and how to manage them
| Drug type | Side effect | What will your doctor do | What you can do |
|---|---|---|---|
| Chemotherapy | Gastrointestinal problems
|
Prescribe
|
|
| Immuno-modulatory drugs, Proteasome inhibitors, some antibodies | Decreased blood counts |
|
|
| Immuno-modulatory drugs | Blood clots |
|
|
| Proteasome inhibitors | Peripheral neuropathy (Pain, numbness or tingling in hands/feet, burning, stumbling, reduced sensation) |
|
|
References:
- Is Multiple Myeloma Genetic? https://www.myelomacrowd.org/myeloma/community/articles/is-multiple-myeloma-genetic. Accessed 8 Apr. 2022.
- “Stem Cell Transplants for Multiple Myeloma | The MMRF.” Themmrf.Org, https://themmrf.org/multiple-myeloma/treatment-options/stem-cell-transplants/. Accessed 7 Apr. 2022.